Lower Jaw Reconstruction for Juvenile Ossifying Fibroma
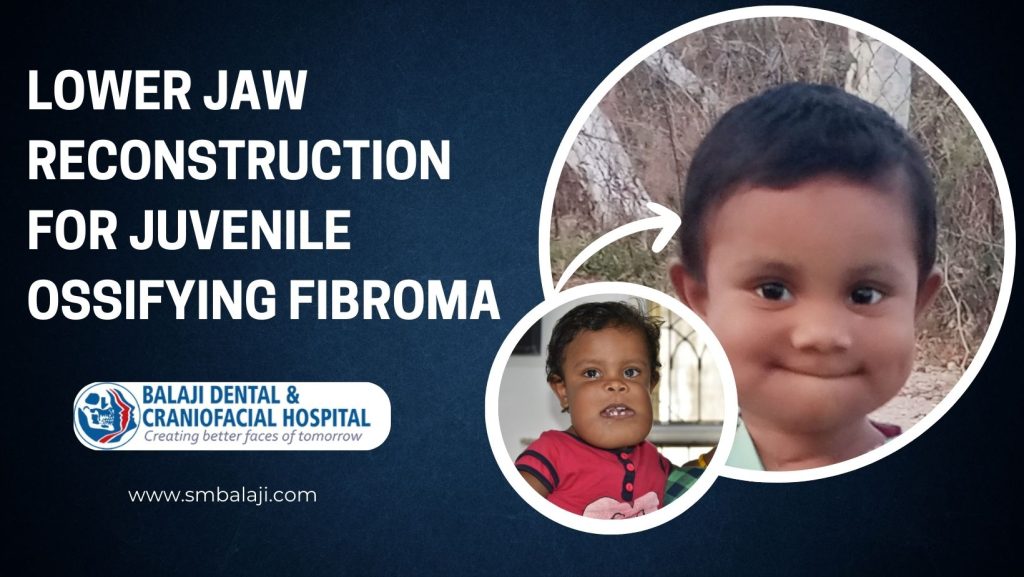
Etiology and Incidence of Juvenile Ossifying Fibroma in Children Juvenile ossifying fibroma is a benign tumor, which demonstrates aggressive expansion. It is quite uncommon and there is aggressive formation of new bone. This results in gross facial deformities of the involved bones, most commonly the jaws. Periodontal Ligaments as the Source for Juvenile Ossifying Fibroma The etiology of this lesion is unknown and it usually arises from the periodontal ligaments. Diagnosis is enabled both through histology and radiographic imaging studies. Imaging studies reveal it to be a radiolucent lesion, which has focal calcifications in the mass. Radiographic and Histologic Composition of the Lesions This lesion comprises of bony tissue, fibrous tissue and a cementum like material. Cementum is the material that lines the surface of the tooth roots. The periodontal ligaments are attached to the cementum and the bone on either end. Involvement of the Mandible as the most Common Site for Lesion The most common site for juvenile ossifying fibroma is the lower jaw. It also occurs in the upper jaw or the maxillary region. Many cases are asymptomatic through some patients have gross disfigurement. Need for Jaw Reconstruction Surgery after Resection of Lesion Some of these lesions are extremely large and require surgery. Surgical resection of these large lesions results in large bony defects. The large bony defects have to be reconstructed using bone grafts and titanium plates. Maxillary osteotomy and mandibular osteotomy are corrective jaw surgery. Performed under general anesthesia by oral and maxillofacial surgeons, they deal with the upper and lower jaw bones. Surgical correction of open bite is obtained through such surgeries. Orthodontic treatment is often performed in conjunction with these surgeries. The jaws and teeth are addressed as a unit during this treatment. This helps to realign the jaw as a whole. The upper teeth and lower teeth alignment is corrected through orthodontic treatment. Tracheostomy tubes are not like ventilators or breathing machines. They are a conduit to enable normal breathing. Certain trauma cases can be life threatening and they are fitted at the front of the neck. They are an integral part of treatment planning for such cases. Little Girl with an Extreme Presentation of Juvenile Ossifying Fibroma This little girl is a case of juvenile ossifying fibroma of both her upper and lower jaws. Her parents had approached many international hospitals for treatment. None of the hospitals were however willing to operate on her. Referral of Complex Pediatric Cases by WorldCF to our Hospital Reaching the end of their tether, they had approached the US-based WorldCF. The World Craniofacial Foundation (WorldCF) is led by Mr. Kenneth Salyer Jr. They have a long standing tie up with Balaji Dental, Craniofacial Hospital & Research Institute. Referral to our Hospital for Jaw Reconstruction Surgery Mr. Salyer had referred her to our hospital for surgery due to our excellent track record. The patient underwent initial diagnostics including imaging studies at our hospital. Confirming the diagnosis of juvenile ossifying fibroma, the treatment plan was formulated. Rare Honor Accorded to only the Finest in the Field Dr. SM Balaji of Balaji Dental, Craniofacial Hospital & Research Institute is a world renowned craniofacial surgeon. He has over 30 years of experience in handling complex cases. Our hospital is the regional affiliate for the WorldCF. A Memorandum of Understanding was signed with Prof. Kenneth E. Salyer. Prof. Salyer is one of the founding fathers of craniofacial surgery. He is also credited with the first successful separation of conjoint twins. Treatment of Complex Syndromic Craniofacial Deformities Many complex surgical cases are referred to us by the WorldCF. Many of these patients had syndromic deformities of the craniofacial complex. These include Crouzon syndrome, Apert syndrome and Treacher-Collins syndrome. Initial Presentation of the Patient at our Hospital Extensive testing was performed on the patient. Detailed examination with pertinent findings was also done. This revealed extreme disfigurement of the upper and lower jaws. The degree of deformity was interfering with her normal activities of daily living. Detailed Diagnostic Studies performed for Best Possible Outcome A 3D CT scan as well as biopsies were also obtained before proceeding with surgery. Detailed planning was performed for the reconstruction of her jaws after resection. Treatment planning was discussed with parents and they consented to surgery. Establishment of Airway through Tracheostomy Airway Tube Bone grafts were first harvested from the patient. These would be utilized for jaw reconstruction. A tracheostomy airway tube was placed following administration of general anesthesia. Once airway was accessed, she underwent segmental resection of her mandible. Insertion of Tracheostomy Airway Tube in Pediatric Patients A tracheostomy airway tube is important for a pediatric patient undergoing major jaw surgery. Child jaw surgery is performed on sized pediatric jaws. A tracheostomy airway tube ensures unimpeded air flow for such patients. Delicate Nature of Jaw Reconstruction Surgery in Small Patients Anesthesiology in child jaw surgery is also best performed by experienced anesthesiologists. All structures are small in pediatric patients and the tissues are also very delicate. Jaw reconstruction surgery also needs a lot of experience for such patients. Jaw Reconstruction Surgery with Child Jaw Surgery The lower jaw defect was reconstructed with the reconstruction plate. This was followed by resection of the lesion from the upper jaw. The bone grafts were then fixed to the reconstruction plate for completion of the lower jaw reconstruction. Successful Recovery from Child Jaw Surgery with Reconstructed Jaw The patient was doing fine and feeding well on the seventh postoperative day after surgery. Her lower facial swelling had also gradually decreased in the postoperative period. Parents were provided detailed instructions on postoperative care for their daughter. Lower Jaw Reconstruction for Juvenile Ossifying Fibroma Click Here to watch the surgery video
Surgical Release of Bilateral Jaw Joint Fusion

Surgical Release of Bilateral Jaw Joint Fusion Probability of Injury to the Temporomandibular Joint from falls Childhood is a time of fun and frolic and a lot of play. This can lead to a lot of bruises and scrapes from falls. Many instances of direct falls on the chin are common. This is the most common cause of injury to the temporomandibular joint (TMJ). Relative Minor Joint Injuries Leading to Complete Bony Ankylosis Many of these falls are minor with only minor pain and discomfort arising in the joint. Initial management is usually through analgesics prescribed by family physicians. Many of the patients are not followed up once there is symptomatic relief from the pain. Classification of TMJ Ankylosis into Fibrous and Bony Ankylosis Even relatively minor injuries can result in bleeding into the jaw joints. This gradually results in fusion of the jaw joints to the skull bones. There are two types of ankylosis of the TMJ. Fibrous ankylosis affords a little movement while bony ankylosis results in immobility of the joint. Patient Suffers a fall to the Chin with Resultant Injury to the Jaw Joints This young boy had suffered an injury to his jaw joints a few years ago. He had fallen on his chin during play at school. A local doctor had prescribed analgesics and he did not have any pain. His parents did not follow up on the possibility of temporomandibular joint injury. Increasing Mouth Opening Limitation and Lower Jaw Retrusion He gradually developed limitation in his mouth opening as well as mandibular retrognathism. This has now reached a point where he now has very limited mouth opening. They presented to a local doctor who explained the condition to them. Initial Diagnosis of Bony Jaw Joint Ankylosis at Hometown Hospital He stated that he had complete bony ankylosis. Explaining that he needed surgical treatment for TMJ, he reiterated the need for expert care. A referral was then made to our hospital for management of his condition. Renowned Jaw Surgery Hospital in the Southeast Asian region Our hospital is a superspecialty jaw surgery hospital. We have won recognition from our peers for being a premier jaw surgery hospital. Treatment of TMJ problems are a hallmark of a good jaw surgery hospital. Dr. SM Balaji of Balaji Dental, Craniofacial Hospital & Research center is a world renowned jaw joint surgeon. He has over 30 years of experience in handling complex cases. Meeting Stringent Requirements for Surgery for TMJ Abnormalities Our hospital is world renowned for our services for surgery for TMJ abnormalities. The range of surgery for TMJ problems include trauma and congenital deformities of the joint. We perform recessive jaw surgery through advancement of the jaw. Recessive Jaw Surgery through Jaw Advancement Surgery Two modalities are usually utilized to perform setback surgery for jaw correction. The most common procedure for recessive jaw surgery is bilateral sagittal split osteotomy. This is effective and recovery is quick in the postsurgical period. We offer a wide range of surgical services for correction of facial deformities. Our hospital is one of the pioneers in the field of facial feminization surgery in India. We perform correction of all congenital and traumatic jaw deformities in our hospital. Orthognathic surgery is a specialized treatment to correct jaw problems. Our hospital is a surgical center of excellence for joint space correction of TMJ disorders. TMJ arthroscopy is a procedure that is used to investigate the tissues of the joint. Conservative treatments include physiotherapy and exercises for the jaw joint. Fibrous ankylosis is caused by scar tissue like fibrous union of the joint. Jaw joint surgical procedures are always performed under general anesthesia. Recovery time is quick from this surgery. Long term exercises are necessary to manage and reduce chronic pain. The oral surgeon is the specialist who deals with upper jaw pain and pain in the jaw joint. Anti-inflammatory medications only provide temporary relief for many cases. Leading Center for Facial Cosmetic Surgery and Facial Plastic Surgery Our hospital is a superspecialty center for correction of nasal deformities. Many patients from across the globe present to our hospital for rhinoplasty correction. Nose correction surgery is technique sensitive. Experienced surgeons provide the best results for such surgeries. Another superspecialty surgery performed in our hospital is microtia ear reconstruction. This surgery is offered in very few surgical centers in our country. The surgery is a two stage surgery performed over a period of three months. First stage of the surgery involves harvesting the fourth, fifth and sixth costal rib cartilages. These are crafted with care to mimic the cartilaginous outer ear structure. This is then carefully placed in an ear pocket crafted at the site of the ear. This is followed by the second stage surgery. The previously placed cartilaginous ear structure is lifted up. The posterior portion of the ear is then addressed through a skin graft. This skin graft is most often harvested from the abdominal region of the patient. Imaging Studies reveal Bilateral Bony Ankylosis of Jaw Joints Imaging studies were obtained including a 3D CT scan and he was examined. There was a thick medial callus of the ankylosed jaw joints. Treatment planning was explained to the parents and they consented to surgery. Release of Ankylosed Jaw Joints with Good Mouth Opening The jaw joints were approached through bilateral submandibular incisions. His bilaterally ankylosed jaw joints were released using a burr. There was greatly increased mouth opening following his surgery of up to 2 inches. Importance of Jaw Exercises in Preventing Relapse of Jaw Ankylosis His parents have been advised to perform rigorous jaw exercises. This would ensure that there was no recurrence of his ankylosis. They expressed understanding of the instructions before discharge from the hospital. Surgical Release of Bilateral Jaw Joint Fusion CLICK HERE TO WATCH THE SURGERY VIDEO
A Triumph Over Adversity: Jaw Reconstruction for Ameloblastoma – A Patient’s Journey
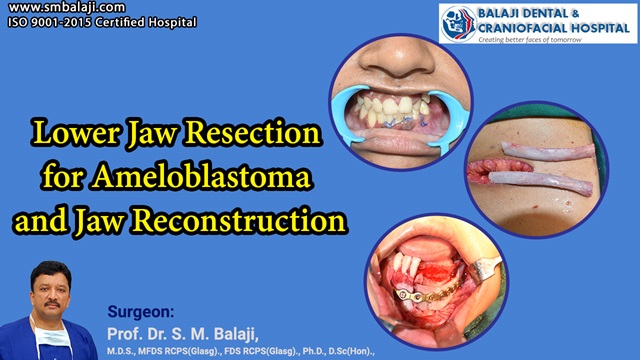
Lower Jaw Resection for Ameloblastoma and Jaw Reconstruction Pathogenesis of Ameloblastoma and Treatment Modes An ameloblastoma is a benign odontogenic tumor that most often arises in the lower jaw. The most common region is the area near the molar teeth. It is often aggressive in nature and causes extensive destruction of the jaw bone. Successful Surgical Treatment of Ameloblastoma with Segmental Resection Segmental jaw resection is the most common surgical mode of treatment of ameloblastoma. The section of affected jaw along with overlying teeth is removed. This results in a large bony defect, which leads to cosmetic and functional compromise. Common Modes of Diagnosis of Ameloblastoma of the Jaw Diagnosis is most commonly through biopsy and imaging studies. It appears as a radiolucent lesion, which is well defined and with scalloped borders. The scalloped borders are caused by the multilocular presentation of the tumor. Histopathological Genesis of the Tumor in the Mandible Ameloblastoma of the jaw arises from the cells that are the precursor to enamel. Occurrence in children can lead to delayed eruption of teeth. Adults often experience loosening of teeth in the region and difficulty with speech. Extensive Destruction of Bony Structure of the Mandible Patients who develop ameloblastoma of the jaw require jaw reconstruction surgery. Jaw bone grafting needs to be performed using rib bone grafts. A time period of six months is allowed to elapse after jaw bone grafting. This allows adequate consolidation of the graft bone. Surgical Specialty Dealing with the Treatment of Ameloblastoma Treatment of ameloblastoma of the jaw is performed by maxillofacial surgeons. This is achieved by segmental resection of the affected segment of the jaw. This is followed by jaw reconstruction surgery. Patients who develop ameloblastoma of the jaw fully recover from their condition. Jaw reconstruction surgery is followed by placement of dental implants. Shade matched ceramic crowns are placed after osseointegration of the implants. Treatment plan with this surgical procedure includes long term correct jaw relationship. A CT scan is obtained before this corrective jaw surgery. All possibilities for side effects are studies to ensure that they do not arise. The soft tissues also play an important role in determining the shape of the face. Relationship between the upper and lower jaw is studied in detail. The bone structure is also analyzed. This will help chose the choice of bone graft material. Bone graft procedures are explained in detail to the patient. Care is also taken to avoid complications such as a postoperative open bite. The gum tissue is also analyzed for postoperative drape. These procedures are always performed under general anesthesia. They also often require orthodontic treatment for correction of tooth alignment. Patients with obstructive sleep apnea have a characteristic profile with receding chins. Successful Rehabilitation of Patients with Full Return to Normalcy Our hospital is a superspecialty oral and craniomaxillofacial surgery hospital. Located in Chennai, India, it has won international acclaim for its surgical services. We address all conditions related to the craniofacial complex. Dr. SM Balaji of Balaji Dental, Craniofacial Hospital & Research Institute is a world renowned craniofacial surgeon. He has over 30 years of experience in handling complex cases. Delivery of healthcare is holistic in nature in our hospital. We believe in the overall wellbeing of the patient. Education is imparted to patients regarding the impact of oral health on overall health. Our approach to treatment came to the fore during the recent COVID-19 pandemic. We have always placed the greatest importance to overall patient wellbeing. Modules were developed to educate patients on reducing their risk to getting infected. Stress was laid on the wear masks, wash hands and maintain distance protocol. We have always had the latest infrastructure regarding asepsis and infection control. Staff were regularly updated on information developed by leading scientists. We were also amongst the first to commence surgeries in our nation. Diligent attention was paid to ensure that patient safety was always ensured. Our untiring efforts won recognition from many quarters across the nation. World Class Amenities at our Superspecialty Surgical Center We have been rendering excellence in surgical care for over three decades now. Our hospital has two state of the art operation theaters with the latest equipment. We also have 24 well-appointed rooms for inpatient admissions. Continuous Medical Education Programs for Staff Members Our medical and paramedical staff are up to date with the latest surgical developments. We are credited with many surgical innovations in the field of craniomaxillofacial surgery. Many Western surgeons apply for viewership in our operation theaters. We keep abreast with the latest developments in the surgical sciences. Jaw bone grafting is exclusively performed using rib grafts. Precise jaw bone grafting requires a high degree of skill and experience. Rib bone grafts are the gold standard for use in jaw bone grafts. Patient Notices Insidious Development of Lower Jaw Swelling This young woman had noticed a swelling involving her left lower jaw for a few months now. She had noticed that it was also painful when chewing and biting. This had begun to alarm her as it kept increasing in size. Diagnosis of Ameloblastoma through Imaging Studies and Biopsy Imaging studies and biopsies were obtained upon presentation at our hospital. This had returned with a diagnosis of ameloblastoma involving the left lower jaw. Treatment planning for jaw reconstruction surgery was explained to the patient. Harvesting Rib Bone Graft for Reconstruction for Jaw Bone Surgery commenced with harvesting of a rib bone graft. This was followed by segmental resection of the lower jaw ameloblastoma. Titanium reconstruction plate and the rib graft was used to reconstruct the bony defect. Successful Rehabilitation of Patient with Dental Implants and Crowns The patient was instructed to return in six months for dental implant placement. This would allow for consolidation of the grafts with surrounding alveolar bone. Another six months would be allowed for osseointegration of the implants. This will be followed by dental crown fixation. Patient’s Reflection In her own words, the patient shares her reflections on the surgical experience,
