Patient with jaw swelling diagnosed as ameloblastoma
The patient is a 35-year-old male from a rural district in Andhra Pradesh, India. He had developed a painful swelling in his lower jaw around 12-14 months ago. Alarmed over this, he had presented at a local oral surgical hospital where imaging studies followed by a biopsy had revealed an ameloblastoma. He had been advised to undergo a mandibulectomy (partial removal of lower jaw bone), which had been performed 6-8 months ago. This had been followed by reconstruction of the jaw with a titanium plate and screws.
However, a month following surgery, the patient had developed drainage of pus from the chin region of the jaw from a nonhealing wound. The titanium plate was exposed through this nonhealing wound along with loose screws. There was also gross asymmetry of the face as a result of the surgery. An illusion of an open bite was also created by the surgery. The patient was facing difficulty with speech and eating. He had then presented again to the same oral surgeon for management of his problems.
The surgeon had tried to set right this problem by tightening the screws and debriding and suturing the wound. This had however only worsened the situation for the patient. Realizing this, the patient sought a second opinion at a different hospital locally. Upon examining the patient, the surgeon had realized the complexity of the presenting problem. He had referred him to our hospital for surgical management and correction of his problems.
Our hospital is a premier center for jaw reconstruction surgery in India. Complicated angle to angle mandibulectomy for ameloblastoma surgery is also routinely performed in our hospital followed by jaw reconstruction.
Clinical presentation of an ameloblastoma
Ameloblastoma is a rare, benign or cancerous tumor arising from the odontogenic epithelium. It occurs more commonly in the lower jaw than the upper jaw. Left unattended, they can cause severe disfigurement and destruction of the involved jaw. They are however rarely malignant or metastatic and progress slowly.
Initial examination and treatment planning at our hospital
Dr SM Balaji, jaw reconstruction surgeon, examined the patient and obtained a detailed history. He then ordered comprehensive imaging studies including a 3D CT scan. Clinical examination revealed multiple open wounds in the chin region with significant extraoral pus discharge. Radiographic evaluation showed significant signs of infected plates and screws.
A comprehensive treatment plan was formulated for the patient. It was explained to the patient that the plates and screws needed to be removed because of the infection. The region of the jaw that had been resected would then be reconstructed. This would be through utilization of another mandibular titanium reconstruction plate and screws along with rib grafts.
This would be followed by placement of dental implants in the bone grafts after sufficient integration of the graft with the jaw bone. The open draining chin wound would also be closed. All this was explained to the patient in detail. The patient expressed agreement with the treatment plan and consented for surgery.
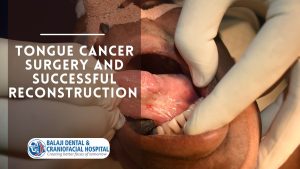
Successful surgical reconstruction of the jaw
Under general anesthesia, a midcrestal incision was made in the left mandible followed by elevation of a mucoperiosteal flap. This exposed the infected mandibular reconstruction plate and screws. These were then removed along with an infected mandibular right second molar. Necrotic soft bone surrounding the infected tooth root and plate screws was also removed. Mandibular reconstruction was then performed using the titanium reconstruction plate and screws.
Following this, an inframammary incision was made to harvest the rib grafts. A Valsalva maneuver was then performed to ensure that there was no perforation into the thoracic cavity. The wound was then closed in layers with sutures.
Bone grafts were then fixed to the titanium reconstruction plates with screws to reconstruct the bony defect in the mandible. This resulted in reestablishment of mandibular contour and symmetry. Also, the necrotic skin and soft tissue in the extraoral wound in the chin that had been draining pus was excised. This was followed by approximation and closure of healthy tissue using sutures.
A period of 4-6 months would be allowed for complete integration of the rib grafts with the mandibular bone. The patient was instructed to return at that time for dental implant surgery. Artificial teeth would be fitted to the dental implants following osseointegration of the implants. An abutment is attached from the implant to each artificial tooth. This would complete total rehabilitation of the patient. The patient was counseled that meticulous gum tissue and oral dental care was needed for long term success of the implants.
Patient expresses complete satisfaction with the surgery
Healing of the surgical wounds was uneventful and the patient recovered completely from the surgery. He was very happy with the outcome of the surgery. Facial symmetry had been reestablished and he was completely pain free.